SUMMARY: Omacetaxine Mepesuccinate (SYNRIBO®) is a first-in-class cephalotaxine and is a semi synthetic purified Homoharringtonine (HHT) compound. HHT is a plant alkaloid derived from Cephalotaxus fortunei, a coniferous bush, also called Japanese Plum Yew. With over 40 years of drug development history since its discovery, SYNRIBO®, unlike Tyrosine Kinase Inhibitors (TKI), is a protein synthesis inhibitor and reduces the levels of multiple Oncoproteins including BCR-ABL, BCL-2, MCL-1 and promotes apoptosis of leukemic stem cells. The following is the pooled data from 2 phase II trials. Treatment population included patients with Chronic Myeloid Leukemia – Chronic Phase (CML-CP), resistant or intolerant to GLEEVEC® (Imatinib) and at least one other TKI such as SPRYCEL® (Dasatinib) and/or TASIGNA® (Nilotinib). All patients had prior treatment with GLEEVEC®, 85% had prior treatment with SPRYCEL® and 59% had prior treatment with TASGNA®. The primary end point was Major Cytogenetic Response (MCyR) and 81 patients with a median age of 59 years were included in this analysis. Treatment consisted of subcutaneous SYNRIBO®, administered at 1.25 mg/m2 twice daily for 14 consecutive days every 4 weeks until response, then for 7 days every 4 weeks as maintenance treatment. The median duration of treatment was 7.5 months. MCyR was noted in 20% of the patients and the median response duration was 17.7 months. Hematologic response was seen in 69% of the patients and the median response duration was 12.2 months. The median failure-free survival was 9.6 months and overall survival was 34 months. The most common grade 3/4 toxicities were cytopenias. The authors concluded that SYNRIBO® has clinical activity in a heavily pretreated population of patients with CML-CP and should therefore be considered for patients with CML-CP with resistance or intolerance to 2 or more TKI’s. By virtue of its mechanism of action, patients with T315I BCR-ABL mutation may potentially benefit from this unique compound. Cortes JE, Nicolini FE, Wetzler M, et al. Clin Lymphoma Myeloma Leuk. 2013;13:584-591.
Month: October 2013
PROSE: Randomized proteomic stratified phase III study of second line erlotinib versus chemotherapy in patients with inoperable non–small cell lung cancer (NSCLC)
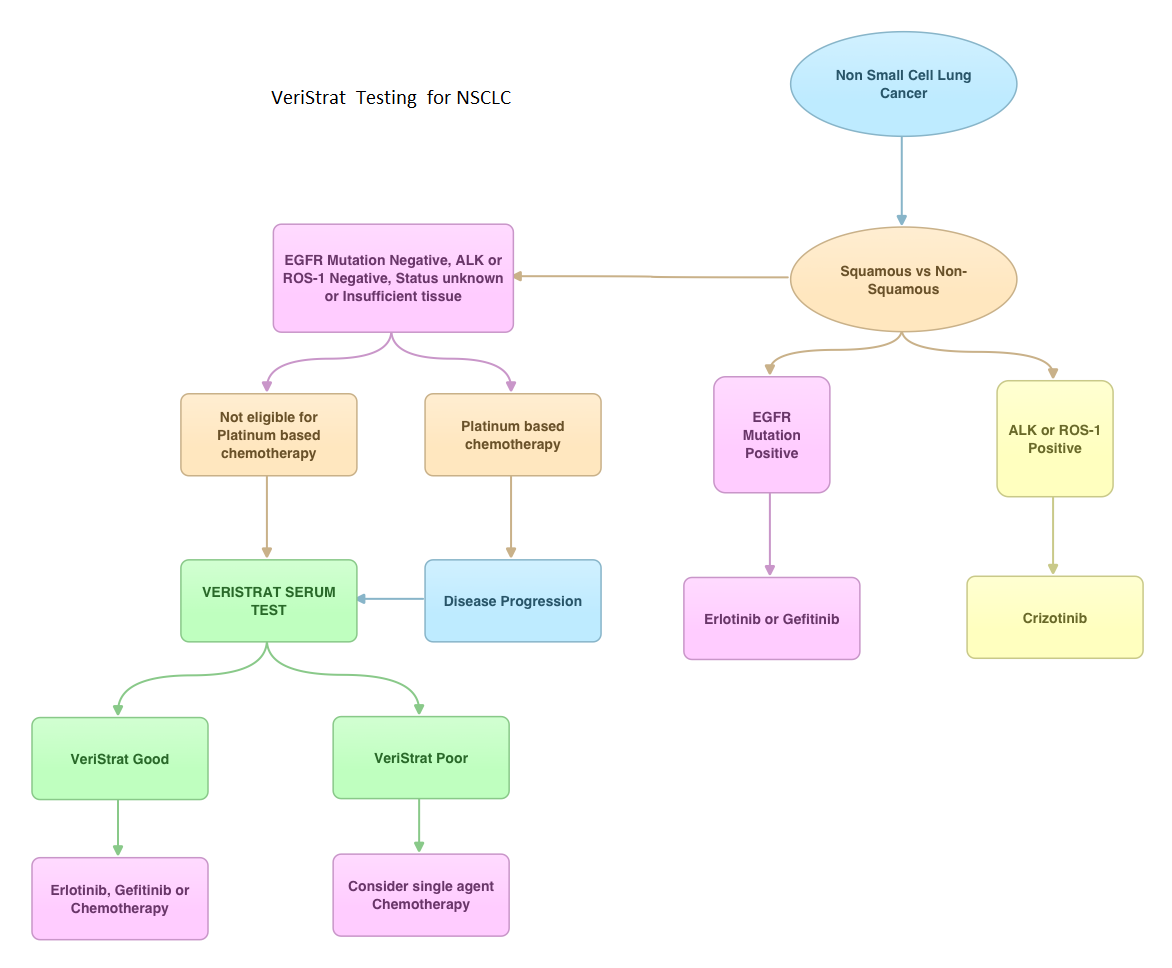
SUMMARY: VeriStrat ® is a clinically validated serum/plasma-based assay, for patients with advanced Non Small Cell Lung Cancer (NSCLC). VeriStrat® is a serum test of prognostic and predictive value that classifies patients as VeriStrat-Good (VS-G) or VeriStrat-Poor (VS-P) based on eight mass spectral peaks or proteomic patterns of the patients serum. Proteomics is the large-scale study of protein structure and functions. VeriStrat® testing is protein based and therefore has no correlation with known genomic biomarkers. It is well established that EGFR-TKIs (Epidermal Growth Factor Receptor-Tyrosine Kinase Inhibitors) are more effective in NSCLC patients with EGFR activating mutations. PROSE is a multicenter, double blind, randomized, VeriStrat® stratified, phase III study. In this trial, over 90% of the patients had no EGFR mutations (EGFR-Wild Type). Two hundred and eighty five (285) patients with advanced NSCLC who had first line treatment regimen with platinum-based therapy were randomly assigned to receive second line chemotherapy (CT) with single agent ALIMTA® (Pemetrexed) or TAXOTERE® (Docetaxel), at standard doses (N=129) or TARCEVA® (Erlotinib) 150 mg po qd (N=134). Patients and study investigators were blinded to the patients VeriStrat® status. Patients were classified as VeriStrat-Good or VeriStrat-Poor based on the VeriStrat® results. Patients in the treatment groups were stratified by age, gender, tumor histology, ECOG-PS and smoking history. Crossover was permitted upon disease progression. The primary objective of the study was to demonstrate differential treatment benefit between TARCEVA® and CT with regards to Overall Survival (OS). Median overall survival (OS) was 9 months for the patients in the CT group and 7.7 months for TARCEVA® group and this was not statistically significant (P=0.3). However when evaluated by VeriStrat® status, CT was beneficial for the VeriStrat-Poor patients compared to TARCEVA®, with significantly better median OS (6.3 vs 3 months, P=0.02). Age, gender, histology (squamous vs non-squamous) and smoking history had no impact on the overall survival. The authors concluded that patients classified as VeriStrat-Poor have better survival with CT than TARCEVA®, whereas patients classified as VeriStrat-Good have similar survival with TARCEVA® and CT. VeriStrat® testing therefore, can help physicians choose between TARCEVA® and CT, for their patients with advanced NSCLC. This test helps physicians identify patients who are likely to have good or poor outcomes after treatment with EGFR inhibitors and thereby can provide valuable insight into whether CT or targeted therapy with TARCEVA®, a EGFR-TKI, is appropriate for their patients with advanced NSCLC, in the second line setting. This information is especially important for patients without an EGFR mutation or for those, whose EGFR mutation status is unknown. Sorlini C, Barni S, Petrelli F, et al. J Clin Oncol 29: 2011 (suppl; abstr TPS214)
PROSE Randomized proteomic stratified phase III study of second line erlotinib versus chemotherapy in patients with inoperable non–small cell lung cancer (NSCLC)
SUMMARY: VeriStrat ® is a clinically validated serum/plasma-based assay, for patients with advanced Non Small Cell Lung Cancer (NSCLC). VeriStrat® is a serum test of prognostic and predictive value that classifies patients as VeriStrat-Good (VS-G) or VeriStrat-Poor (VS-P) based on eight mass spectral peaks or proteomic patterns of the patients serum. Proteomics is the large-scale study of protein structure and functions. VeriStrat® testing is protein based and therefore has no correlation with known genomic biomarkers. It is well established that EGFR-TKIs (Epidermal Growth Factor Receptor-Tyrosine Kinase Inhibitors) are more effective in NSCLC patients with EGFR activating mutations. PROSE is a multicenter, double blind, randomized, VeriStrat® stratified, phase III study. In this trial, over 90% of the patients had no EGFR mutations (EGFR-Wild Type). Two hundred and eighty five (285) patients with advanced NSCLC who had first line treatment regimen with platinum-based therapy were randomly assigned to receive second line chemotherapy (CT) with single agent ALIMTA® (Pemetrexed) or TAXOTERE® (Docetaxel), at standard doses (N=129) or TARCEVA® (Erlotinib) 150 mg po qd (N=134). Patients and study investigators were blinded to the patients VeriStrat® status. Patients were classified as VeriStrat-Good or VeriStrat-Poor based on the VeriStrat® results. Patients in the treatment groups were stratified by age, gender, tumor histology, ECOG-PS and smoking history. Crossover was permitted upon disease progression. The primary objective of the study was to demonstrate differential treatment benefit between TARCEVA® and CT with regards to Overall Survival (OS). Median overall survival (OS) was 9 months for the patients in the CT group and 7.7 months for TARCEVA® group and this was not statistically significant (P=0.3). However when evaluated by VeriStrat® status, CT was beneficial for the VeriStrat-Poor patients compared to TARCEVA®, with significantly better median OS (6.3 vs 3 months, P=0.02). Age, gender, histology (squamous vs non-squamous) and smoking history had no impact on the overall survival. The authors concluded that patients classified as VeriStrat-Poor have better survival with CT than TARCEVA®, whereas patients classified as VeriStrat-Good have similar survival with TARCEVA® and CT. VeriStrat® testing therefore, can help physicians choose between TARCEVA® and CT, for their patients with advanced NSCLC. This test helps physicians identify patients who are likely to have good or poor outcomes after treatment with EGFR inhibitors and thereby can provide valuable insight into whether CT or targeted therapy with TARCEVA®, a EGFR-TKI, is appropriate for their patients with advanced NSCLC, in the second line setting. This information is especially important for patients without an EGFR mutation or for those, whose EGFR mutation status is unknown. Sorlini C, Barni S, Petrelli F, et al. J Clin Oncol 29: 2011 (suppl; abstr TPS214)
VERISTRAT® Testing – A novel approach to NSCLC
VeriStrat®, a serum based proteomic assay can help physicians identify patients who are likely to have good or poor outcomes after treatment with EGFR inhibitors and thereby can provide valuable insight into whether chemotherapy or targeted therapy with TARCEVA®, a EGFR-TKI, is appropriate for their patients with advanced NSCLC, in the second line setting. This information is especially important for patients without an EGFR mutation or for those, whose EGFR mutation status is unknown. In the PROSE trial, patients classified as VeriStrat-Poor have better survival with chemotherapy than TARCEVA®, whereas patients classified as VeriStrat-Good have similar survival with TARCEVA® and chemotherapy. This data was presented at the 2013 ASCO meeting.
Single-Agent Lenalidomide in Patients With Mantle-Cell Lymphoma Who Relapsed or Progressed After or Were Refractory to Bortezomib Phase II MCL-001 (EMERGE) Study
SUMMARY: In the MCL-001 trial, 134 patients with relapsed or refractory Mantle Cell Lymphoma (MCL) were enrolled. These patients had received prior treatment with RITUXAN® (Rituximab), CYTOXAN® (Cyclophosphamide), an Anthracycline and VELCADE® (Bortezomib) alone or in combination. The median age was 67 years and patients received a median of 4 prior therapies for MCL. Treatment consisted of Lenalidomide (REVLIMID®) 25 mg given orally on days 1 thru 21, of a 28 day cycle. Treatment was continued until disease progression or treatment intolerance. The primary efficacy endpoints were overall response rate (ORR) and duration of response (DOR). The secondary endpoints included Complete Response (CR), Progression Free Survival (PFS) and Overall Survival (OS). The ORR was 28% with a CR of 7% and the median DOR for those who responded to REVLIMID® was 16.6 months. The median PFS was 4 months and the median OS was 19 months.The most common grade 3-4 adverse reactions were cytopenias, fatigue, dyspnea and diarrhea. The authors concluded that REVLIMID® is the first drug to receive approval for the treatment of MCL since VELCADE® was approved for this disease in 2006 and gives one additional option for MCL patients, refractory to VELCADE®. Goy A, Sinha R, Williams ME, Besisik SK et al. J Clin Oncol 2013;31:3688-3695
Phase III Study of Afatinib or Cisplatin Plus Pemetrexed in Patients With Metastatic Lung Adenocarcinoma With EGFR Mutations
SUMMARY: GILOTRIF® (Afatinib) is an oral, irreversible blocker of the ErbB family which includes EGFR (ErbB1), HER2 (ErbB2), ErbB3 and ErbB4. The approval of GILOTRIF® was based on a multi-center, international, open-label, randomized, phase III trial, in which 345 patients with Stage IIIB (wet)/IV lung adenocarcinoma, with tumors demonstrating Epidermal Growth Factor Receptor (EGFR) exon 19 deletions or exon 21 (L858R) substitution mutations, as detected by an FDA-approved test, were enrolled in a 2:1 ratio. Patients were randomized to receive GILOTRIF® 40 mg orally once daily (n=230) or ALIMTA® (Pemetrexed)/Cisplatin (n=115) given every 21 days for up to six cycles. Patients were stratified according to EGFR mutation status (exon 19 deletion vs. exon 21 L858R vs. ‘other’) and race (Asian vs. non-Asian). The primary endpoint was Progression Free Survival (PFS). The median PFS in the GILOTRIF® group was 11.1 months and 6.9 months in the chemotherapy group (HR= 0.58, P<0.001). In patients whose tumors demonstrated EGFR mutations, the median PFS was 13.6 months in the GILOTRIF® arm and 6.9 months in the chemotherapy arm (HR= 0.47, P<0.001). Objective response rates were 56% and 23% in the GILOTRIF® and chemotherapy groups respectively (P=0.001). There was no statistically significant difference in overall survival between the two treatment groups. The most frequent adverse reactions in the GILOTRIF® group were skin rash, pruritus, stomatitis, diarrhea and decreased appetite. The authors concluded that GILOTRIF® is better than chemotherapy in the first line treatment of EGFR mutant Non Small Cell Lung Cancer patients. However, it remains to be seen if this agent is superior to TARCEVA® (Erlotinib) and IRESSA® (Gefitinib). Sequist LV, Yang JC, Yamamoto N, et al. J Clin Oncol 2013;31:3327-3334
Use of Molecular Biomarkers to Inform Adjuvant Therapy for Colon Cancer
SUMMARY: The role of adjuvant chemotherapy in patients with stage III ColoRectalCancer (CRC) has been well established, with improvement in Disease Free Survival (DFS) and Overall Survival (OS). The same however, cannot be stated for patients with Stage II CRC. Several Prognostic (outcome regardless of specific treatment) and Predictive (benefit from a specific therapy) molecular biomarkers have been developed to help make treatment decisions which include MSI (MicroSatellite Instability), LOH 18q (Loss of heterozygosity on the long arm of chromosome 18), P53, TS (Thymidylate Synthase), KRAS, BRAF, ERCC1 (Excision Repair Cross-Complementation group 1), Oncotype DX and Coloprint. Even though LOH 18q, P53, TS, KRAS, BRAF and ERCC1 are of prognostic value, they presently do not provide clinical utility in the management of early stage CRC. The biomarkers of interest are MSI, Oncotype DX Colon Cancer Assay and ColoPrint. MMR and MSI: MSI is the hallmark of defective/deficient DNA MisMatchRepair (MMR) system and develops following a germline mutation in one of the MMR genes. The MMR gene system consists of several proteins which are responsible for surveillance and correction of DNA errors. These genes include MLH1, MSH2, MSH6, PMS2 and EPCAM. MSI-high (MSI-H, MMR deficient) is actually a good prognostic marker in early stage CRC, with less likelihood of lymph node involvement, systemic metastases and with improved survival. These patients do not benefit from DNA inhibiting anti-metabolites such as 5-FluoroUracil (5-FU). In fact, treatment with 5-FU could be detrimental, whereas they may be more responsive to Irinotecan. This is in contrast to early stage CRC patients with tumors that are MicroSatelliteStable (MSS) or MSI-low (MSI-L) and MMR proficient, who benefit from 5-FU based adjuvant chemotherapy with significantly improved DFS. It should be noted that the prognosis for patients with early stage CRC, whose tumors harbor V600E BRAF mutation and are MSI-H, is similar to CRC patients with MSS tumors. MSI is a genetic marker of Lynch Syndrome (Hereditary Nonpolyposis Colorectal Carcinoma – HNPCC) and approximately 15% of sporadic CRC share the genetics of Lynch Syndrome and are MSI-H and MMR-deficient. By evaluating the MMR/MSI status of a CRC patient, a clinician may be able to assess a patient’s prognosis, predict response to therapy and detect Lynch’s Syndrome, which constitutes about 3-5% of CRC cases. MSI is a functional assay and can be detected by PCR whereas ImmunoHistoChemistry (IHC) can confirm the presence or absence of MMR proteins.
ONCOTYPE DX COLON CANCER ASSAY: Oncotype DX Colon Cancer assay is a multigene expression assay and evaluates genes in the patient’s tumor, using paraffin slides. It consists of 7 potential recurrence genes and 5 internal reference genes and has been clinically validated from three prospective trials, to assess risk of recurrence, in patients with Stage II and III CRC. The Oncotype DX colon cancer assay is able to prognosticate the risk of recurrence of a particular CRC tumor but unlike the Oncotype DX assay for Breast Cancer, is unable to predict clinical benefit from adjuvant chemotherapy.
COLOPRINT: This assay uses an18 gene expression profile and requires fresh tissue. This assay is also able to assess the risk of recurrence in Stage II CRC but is unable to predict the benefit from adjuvant chemotherapy.
In summary, testing for MSI should be performed in all patients with Stage II CRC. Genetic signatures derived from Oncotype Dx Colon Cancer assay and ColoPrint may have limited clinical value for patients with early stage CRC. NCCN guidelines recommend adjuvant chemotherapy for high risk Stage II CRC. High risk for recurrence is defined as tumors that are poorly differentiated (except those tumors that are MSI-H), lymphovascular invasion, perineural invasion, bowel obstruction, localized perforation, close, indeterminate or positive margins and examination of less than 12 lymph nodes. Mettu NB, Hurwitz H and Hsu DS. Oncology 2013;27:746-754
PERJETA® combination Improves Response Rates
The FDA on September 30, 2013 approved PERJETA® for use in combination with HERCEPTIN® (Trastuzumab) and TAXOTERE® (Docetaxel) for the neoadjuvant treatment of patients with HER2-positive, locally advanced, inflammatory, or early stage breast cancer. The accelerated approval by the FDA was based solely on the improved pCR rate with the three drug combination with no demonstrable improvement in event-free survival or overall survival. A confirmatory phase III trial is underway, with results expected in 2016. One would hope that the complete response rates would translate into improved survival. Stay tuned.
Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere) a randomised multicentre, open-label, phase 2 trial
SUMMARY: PERJETA® (Pertuzumab) is a recombinant, humanized, monoclonal antibody that binds to the HER2 dimerization domain and prevents the dimerization of HER2 with other HER receptors, ie. HER3, HER1 and HER4. HERCEPTIN® (Trastuzumab) is a monoclonal antibody that specifically targets the HER2 receptor and blocks the downstream signalling pathways. The accelerated approval of PERJETA® for the neoadjuvant treatment of breast cancer was based on a randomized, multicenter, open-label, phase II trial, in which 417 patients with HER2-positive, operable, locally advanced or inflammatory breast cancer (T2-4d), were randomly assigned to receive preoperative therapy with either HERCEPTIN® plus TAXOTERE® (Docetaxel), PERJETA® plus HERCEPTIN® and TAXOTERE®, PERJETA® plus HERCEPTIN® or PERJETA® plus TAXOTERE®. Patients in the three drug group received preoperative therapy with PERJETA®, HERCEPTIN® and TAXOTERE® every 3 weeks for a total of 4 cycles and following surgery, all patients received 3 cycles of Fluorouracil, ELLENCE® (Epirubicin), and CYTOXAN® (Cyclophosphamide) – (FEC) IV every 3 weeks and HERCEPTIN® was continued every 3 weeks for a total of one year of therapy. The primary endpoint was pathological Complete Response (pCR) rate defined as the absence of invasive cancer in the breast. The FDA definition of pCR is the absence of invasive cancer in the breast and lymph nodes. All treatment groups were well balanced. Seven percent of patients had inflammatory breast cancer, 32% had locally advanced cancer and 70% had clinically node-positive breast cancer. Forty-seven percent of the patients had hormone receptor-positive disease. The FDA defined pCR rates were 39.3% in the PERJETA® plus HERCEPTIN® and TAXOTERE® group and 21.5% in the HERCEPTIN® plus TAXOTERE® group P=0.0063). Of Interest, the pCR rates in the three drug group were lower in patients with hormone receptor positive tumors compared to patients with hormone receptor negative tumors. The most common adverse events in the three drug group were alopecia, diarrhea, nausea and neutropenia. The accelerated approval by the FDA was based solely on the improved pCR rate with the three drug combination with no demonstrable improvement in event-free survival or overall survival. A confirmatory phase III trial is underway, with results expected in 2016. Gianni L, Pienkowski T, Im YH, et al. Lancet Oncol. 2012;13:25-32
ABRAXANE® TO THE RESCUE
The recent approval by the FDA of ABRAXANE® in combination with GEMZAR® (Gemcitabine) for the first line treatment of patients with metastatic Adenocarcinoma of the Pancreas gives the Oncology Health Care Providers a much needed option to treat this group of patients. With a significant improvement in the Overall Survival, Progression Free Survival and Response Rates, ABRAXANE® combination will very likely replace the more toxic FOLFIRI regimen by virtue of its efficacy and tolerability.
