SUMMARY: It is estimated that in the US, approximately 76,000 new cases of melanoma will be diagnosed and close to 8000 individuals will die of the disease, in 2014. The incidence of melanoma has been on the rise for the past three decades. Unlike other malignancies, the role of chemotherapy for the treatment of melanoma has been limited. Treatment of advanced melanoma with immunotherapy using a cytokine, Interleukin-2 (IL-2), produced by T cells during an immune response, was first explored in the mid 1970’s. Durable responses were noted in a very small percentage of patients but this was associated with significant toxicities. This however opened the doors for the development of various immunotherapies with a better understanding of the Immune checkpoints. Immune checkpoints are cell surface inhibitory proteins/receptors that harness the immune system and prevent uncontrolled immune reactions. Survival of cancer cells in the human body may be to a significant extent, related to their ability to escape immune surveillance, by inhibiting T lymphocyte activation . The T cells of the immune system play a very important role in modulating the immune system.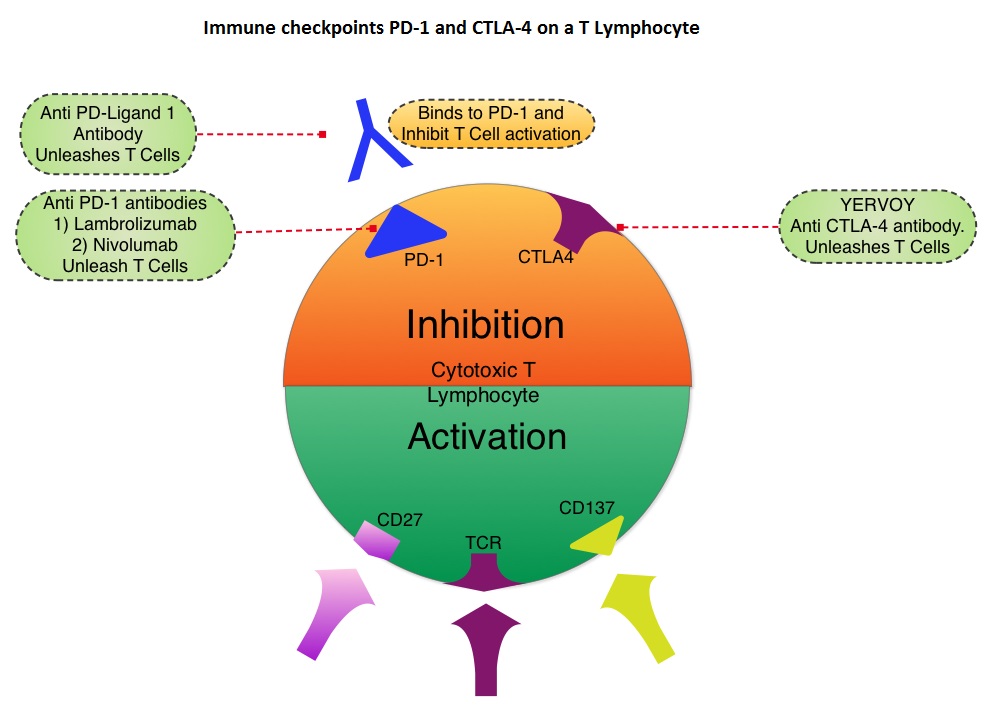 Under normal circumstances, inhibition of an intense immune response and switching off the T cells of the immune system, is an evolutionary mechanism and is accomplished by Immune checkpoints or gate keepers. With the recognition of Immune checkpoint proteins and their role in suppressing antitumor immunity, antibodies are being developed that target the membrane bound inhibitory Immune checkpoint proteins/receptors such as CTLA-4 (Cytotoxic T-Lymphocyte Antigen 4, also known as CD152), PD-1(Programmed cell Death 1), etc. By doing so, one would expect to unleash the T cells, resulting in T cell proliferation, activation and a therapeutic response. The first immune checkpoint protein to be clinically targeted was CTLA-4. YERVOY® (Ipilimumab), an antibody that blocks Immune checkpoint protein/receptor CTLA- 4, has been shown to prolong overall survival in patients with previously treated, unresectable or metastatic melanoma. In a previous publication, the authors reported the efficacy results of Nivolumab, a PD-1 targeted, fully human, immunoglobulin G4 monoclonal antibody, which demonstrated an objective response in 20% – 25% of patients with advanced Non Small Cell Lung Cancer, Melanoma and Renal Cell Carcinoma, with favorable toxicities. In this article, the authors reported the outcomes in 107 patients with advanced metastatic melanoma, from the pooled cohort of patients, enrolled between 2008 and 2012. Two thirds of these patients had at least 2 prior treatments, for their advanced disease. These patients received Nivolumab IV, once every 2 weeks, given in an outpatient setting, for up to 96 weeks. Patients were evaluated for Overall Survival, long term safety with treatment and response duration after the treatment was discontinued. The median Overall Survival in those treated with Nivolumab was 16.8 months and 1 and 2-year survival rates were 62% and 43%, respectively. This survival benefit is comparable to that seen following treatment with other agents that are presently available for this patient population, such as YERVOY® (Ipilimumab), ZELBORAF® (Vemurafenib) and combination of BRAF and MEK inhibitors. BRAF mutational status did not impact efficacy of Nivolumab. About 30% of the patients had objective responses and the median response duration was 2 years. The authors hypothesize that the ongoing tumor response following Nivolumab discontinuation, and unlike following chemotherapy, may be due to PD-1 blockade, resulting in the establishment of immune memory response, as is seen after antigen exposure against specific infectious organisms. The most common adverse events of any grade were fatigue, rash and diarrhea. These toxicities were not cumulative. The authors concluded that Nivolumab improved Overall Survival in patients with advanced melanoma and the clinical benefit was durable and persisted even after the drug was discontinued. Studies are underway combining Nivolumab with a different checkpoint inhibitor, YERVOY®. The synergy between these two agents may result in even better outcomes. Topalian SL, Sznol M, McDermott DF, et al. J Clin Oncol 2014;32:1020-1030
Under normal circumstances, inhibition of an intense immune response and switching off the T cells of the immune system, is an evolutionary mechanism and is accomplished by Immune checkpoints or gate keepers. With the recognition of Immune checkpoint proteins and their role in suppressing antitumor immunity, antibodies are being developed that target the membrane bound inhibitory Immune checkpoint proteins/receptors such as CTLA-4 (Cytotoxic T-Lymphocyte Antigen 4, also known as CD152), PD-1(Programmed cell Death 1), etc. By doing so, one would expect to unleash the T cells, resulting in T cell proliferation, activation and a therapeutic response. The first immune checkpoint protein to be clinically targeted was CTLA-4. YERVOY® (Ipilimumab), an antibody that blocks Immune checkpoint protein/receptor CTLA- 4, has been shown to prolong overall survival in patients with previously treated, unresectable or metastatic melanoma. In a previous publication, the authors reported the efficacy results of Nivolumab, a PD-1 targeted, fully human, immunoglobulin G4 monoclonal antibody, which demonstrated an objective response in 20% – 25% of patients with advanced Non Small Cell Lung Cancer, Melanoma and Renal Cell Carcinoma, with favorable toxicities. In this article, the authors reported the outcomes in 107 patients with advanced metastatic melanoma, from the pooled cohort of patients, enrolled between 2008 and 2012. Two thirds of these patients had at least 2 prior treatments, for their advanced disease. These patients received Nivolumab IV, once every 2 weeks, given in an outpatient setting, for up to 96 weeks. Patients were evaluated for Overall Survival, long term safety with treatment and response duration after the treatment was discontinued. The median Overall Survival in those treated with Nivolumab was 16.8 months and 1 and 2-year survival rates were 62% and 43%, respectively. This survival benefit is comparable to that seen following treatment with other agents that are presently available for this patient population, such as YERVOY® (Ipilimumab), ZELBORAF® (Vemurafenib) and combination of BRAF and MEK inhibitors. BRAF mutational status did not impact efficacy of Nivolumab. About 30% of the patients had objective responses and the median response duration was 2 years. The authors hypothesize that the ongoing tumor response following Nivolumab discontinuation, and unlike following chemotherapy, may be due to PD-1 blockade, resulting in the establishment of immune memory response, as is seen after antigen exposure against specific infectious organisms. The most common adverse events of any grade were fatigue, rash and diarrhea. These toxicities were not cumulative. The authors concluded that Nivolumab improved Overall Survival in patients with advanced melanoma and the clinical benefit was durable and persisted even after the drug was discontinued. Studies are underway combining Nivolumab with a different checkpoint inhibitor, YERVOY®. The synergy between these two agents may result in even better outcomes. Topalian SL, Sznol M, McDermott DF, et al. J Clin Oncol 2014;32:1020-1030
Month: April 2014
ARZERRA® combination for Frontline Treatment of CLL
The FDA on April 17, 2014 approved ARZERRA® (Ofatumumab) in combination with LEUKERAN® (Chlorambucil), for the treatment of previously untreated patients with Chronic Lymphocytic Leukemia (CLL), for whom FLUDARA® (Fludarabine) based therapy is considered inappropriate. ARZERRA® is a second generation fully human IgG 1 monoclonal antibody and unlike RITUXAN® (Rituximab) which is a chimeric monoclonal antibody, targets a different region (different epitope) of the CD20 molecule. The combination of ARZERRA® given along with LEUKERAN® significantly improved Progression Free Survival, Response Rates and duration of response, compared to single agent LEUKERAN®. ARZERRA® in combination with LEUKERAN® is a clinically important milestone, in the management of elderly patients with CLL.
Chemotherapy for isolated locoregional recurrence of breast cancer (CALOR) a randomised trial
SUMMARY:It has been well recognized that patients with Breast Cancer with Isolated LocoRegional Recurrences (ILRR), without evidence of distant metastasis, are at a high risk of developing subsequent distant metastasis and may have poor outcomes, in spite of surgical resection of the ILRR. The role of systemic chemotherapy following surgery in this patient population has remained unclear although hormonal intervention in ER positive patients demonstrated disease free survival benefit. To address this question, three cooperative groups, The International Breast Cancer Study Group (IBCSG), Breast International Group (BIG) and NSABP collaborated and conducted this study to find out whether adjuvant chemotherapy improves the outcome of patients with ILRR following surgical resection. In this multicenter trial, 162 patients were randomly assigned to receive chemotherapy (N=85) or no chemotherapy (N=77). Eligible patients had histologically proven first ILRR resected and radiotherapy was recommended for all patients, but was mandated for those with microscopically involved surgical margins. All patients with ER or PR positive recurrent tumors received endocrine therapy and patients randomized to the chemotherapy group received at least two standard cytotoxic drugs (investigators choice) for 3-6 months. Both treatment groups were well balanced, and hormone receptor status was positive in 68% of the patients belonging to each group. The primary endpoint was Disease Free Survival and secondary endpoints included Overall Survival. The five year Disease Free Survival in the adjuvant chemotherapy group was 69% compared with 57% in the no chemotherapy group (HR=0.59, P=0.046). The five year overall survival was also significantly longer in the chemotherapy group compared to the no chemotherapy group (88% vs 76%, HR=0.41, P=0.024). With regards to the chemotherapy benefit based on hormone receptor status, patients with hormone receptor negative ILRR, had a longer Disease Free Survival with adjuvant chemotherapy (P=0.046). The authors concluded that adjuvant chemotherapy significantly improves Disease Free and Overall Survival in Breast Cancer patients with ILRR. This benefit is even more so, in those with ER negative ILRR. Adjuvant chemotherapy should therefore be considered in this patient population. Aebi S, Gelber S, Anderson SJ, et al. The Lancet Oncology 2014;15:156-163
Ofatumumab + Chlorambucil versus Chlorambucil alone in Patients with Untreated Chronic Lymphocytic Leukemia (CLL) Results of the Phase III Study Complement 1 (OMB110911)
SUMMARY: The American Cancer Society's estimates that approximately 15,720 new cases of chronic lymphocytic leukemia (CLL) will be diagnosed in 2014 and approximately 4600 patients will die from the disease. CLL is a disease of the elderly and the average age at the time of diagnosis is 72 years. Majority of these patients have associated comorbidities and would be considered inappropriate for Fludarabine (FLUDARA®) based therapy. COMPLEMENT 1 is a randomized, open-label, multicenter, phase III trial in which Ofatumumab (ARZERRA®) in combination with Chlorambucil (LEUKERAN®) was compared to single agent LEUKERAN®. ARZERRA® is a second generation fully human IgG 1 monoclonal antibody. Unlike Rituximab (RITUXAN®) which is the chimeric monoclonal antibody, ARZERRA® targets a different region (different epitope) of the CD20 molecule. To go back to basics, several antigen molecules are expressed on the surface of normal B cells. Majority of these antigens are involved in cell growth, proliferation, differentiation, immune regulation and complement activation. The various stages of B cell development include hematopoietic stem cell, lymphoid stem cell, Pro B cell, Pre B cell, Immature B cell and Mature B-cell, Activated B cell, Memory B cell and Plasma cell. The CD20 molecule is expressed at specific stages of B cell development (Pre B cell stage to Mature B lymphocyte stage) and on malignant B cells. This molecule however is not expressed on hematopoietic stem cells and plasma cells. As such, targeting CD20 with therapeutic monoclonal antibodies spares the Pro B cell which is a precursor of Pre B cell and this along with intact hematopoietic stem cell facilitates post treatment recovery of B cells. As the plasma cells are spared as well, serum IgG levels are maintained. Monoclonal antibodies targeting CD20 destroy CD20 positive B cells by 3 different mechanisms. They include Antibody Dependent Cellular Cytotoxicity (ADCC), Complement Dependent Cytotoxicity (CDC) and programmed cell death (Apoptosis).
Monoclonal antibodies targeting CD20 destroy CD20 positive B cells by 3 different mechanisms. They include Antibody Dependent Cellular Cytotoxicity (ADCC), Complement Dependent Cytotoxicity (CDC) and programmed cell death (Apoptosis).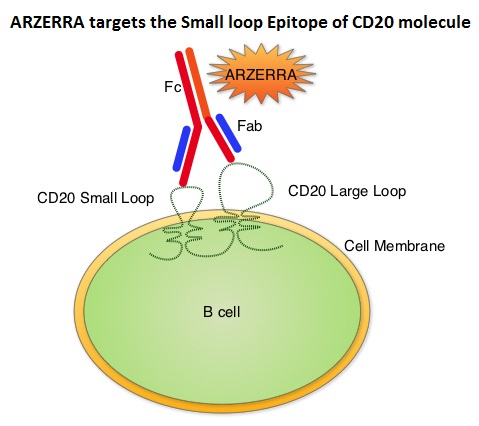 Unlike RITUXAN®, ARZERRA® targets the Small loop epitope of CD20 molecule which is proximal to the B cell membrane and this has been shown to be associated with highly efficient cell lysis through complement dependent cytotoxicity. So, compared to RITUXAN®. ARZERRA® has stronger CDC, similar ADCC and does not appear to induce Apoptosis. In this study, 447 CLL patients for whom FLUDARA® based therapy was considered to be inappropriate due to age and comorbidities, were randomly assigned 1:1 to receive either ARZERRA® in combination with LEUKERAN® or LEUKERAN® alone. ARZERRA® was given as an IV infusion at a dose of 300 mg on Cycle 1, Day 1, 1000 mg on Cycle 1, Day 8 and 1000 mg administered on Day 1 of all subsequent 28 day cycles. LEUKERAN® was given at a dose of 10 mg/m2 orally on Days 1 to 7 every 28 days in both treatment groups. The median age was 69 years and majority of the patients had 2 or more comorbidities. The primary endpoint of this study was Progression Free Survival (PFS) and secondary endpoints included Overall Response Rate (ORR), Overall Survival (OS) and safety. The median number of cycles in both treatment groups was 6. The median PFS was 22.4 months for patients receiving ARZERRA® in combination with LEUKERAN® compared with 13.1 months for those receiving single agent LEUKERAN® (HR=0.57, P< 0.001). The ORR was higher with the combination regimen versus single agent LEUKERAN® (82% vs 69%, P=0.001) and 37% of patients in the combination arm were MRD negative. The median OS for the combination group was not reached. The majority of adverse reactions were Grade 2 or lower, in both of the treatment arms and included infusion reactions, neutropenia, asthenia, headache, herpes simplex, lower respiratory tract infections, arthralgia and upper abdominal pain. The authors concluded that ARZERRA® in combination with LEUKERAN® is a clinically important milestone, in the management of elderly patients with CLL, who are considered inappropriate for FLUDARA® based therapy. Hillmen P, Robak T, Janssens A, et al. Blood 2013;122: Abstract#528
Unlike RITUXAN®, ARZERRA® targets the Small loop epitope of CD20 molecule which is proximal to the B cell membrane and this has been shown to be associated with highly efficient cell lysis through complement dependent cytotoxicity. So, compared to RITUXAN®. ARZERRA® has stronger CDC, similar ADCC and does not appear to induce Apoptosis. In this study, 447 CLL patients for whom FLUDARA® based therapy was considered to be inappropriate due to age and comorbidities, were randomly assigned 1:1 to receive either ARZERRA® in combination with LEUKERAN® or LEUKERAN® alone. ARZERRA® was given as an IV infusion at a dose of 300 mg on Cycle 1, Day 1, 1000 mg on Cycle 1, Day 8 and 1000 mg administered on Day 1 of all subsequent 28 day cycles. LEUKERAN® was given at a dose of 10 mg/m2 orally on Days 1 to 7 every 28 days in both treatment groups. The median age was 69 years and majority of the patients had 2 or more comorbidities. The primary endpoint of this study was Progression Free Survival (PFS) and secondary endpoints included Overall Response Rate (ORR), Overall Survival (OS) and safety. The median number of cycles in both treatment groups was 6. The median PFS was 22.4 months for patients receiving ARZERRA® in combination with LEUKERAN® compared with 13.1 months for those receiving single agent LEUKERAN® (HR=0.57, P< 0.001). The ORR was higher with the combination regimen versus single agent LEUKERAN® (82% vs 69%, P=0.001) and 37% of patients in the combination arm were MRD negative. The median OS for the combination group was not reached. The majority of adverse reactions were Grade 2 or lower, in both of the treatment arms and included infusion reactions, neutropenia, asthenia, headache, herpes simplex, lower respiratory tract infections, arthralgia and upper abdominal pain. The authors concluded that ARZERRA® in combination with LEUKERAN® is a clinically important milestone, in the management of elderly patients with CLL, who are considered inappropriate for FLUDARA® based therapy. Hillmen P, Robak T, Janssens A, et al. Blood 2013;122: Abstract#528
ARZERRA® (Ofatumumab)
ARZERRA® (Ofatumumab): The FDA on April 17, 2014 approved ARZERRA® in combination with LEUKERAN® (Chlorambucil), for the treatment of previously untreated patients with Chronic Lymphocytic Leukemia (CLL), for whom FLUDARA® (Fludarabine) based therapy is considered inappropriate. ARZERRA® first received accelerated approval in 2009, for the treatment of patients with CLL, refractory to FLUDARA® and CAMPATH® (Alemtuzumab). ARZERRA® injection is given as an intravenous infusion and is a product GlaxoSmithKline.
ZYTIGA® improves survival without impacting Quality of Life in CRPC
In a recent article published in The Lancet Oncology, ZYTIGA® (Abiraterone) given along with prednisone delayed patient-reported pain progression and deterioration of Quality of Life in chemotherapy-naive patients with metastatic Castrate Resistant Prostate Cancer (CRPC). This was accomplished without compromising efficacy, which was survival benefit. This is relevant because, patients with Prostate Cancer in general are elderly and it is important that any treatment intervention in this patient population with asymptomatic or mildly symptomatic CRPC improves overall survival without negatively impacting Quality of Life.
Neoadjuvant therapy for rectal cancer Mature results from NSABP protocol R-04
SUMMARY: The American Cancer Society's estimates 40,000 new cases of rectal cancer in the United States for 2014. Rectal cancer diagnosed at an early stage such as Stage II (T3-T4, N0) or Stage III (Node positive disease without distant metastases) is potentially curable with a combination of neoadjuvant (preoperative) chemoradiation, surgery and postoperative chemotherapy. Unlike colon cancer, the risk of locoregional recurrence is high in rectal cancer due to its close proximity to the surrounding pelvic organs and difficulty in obtaining a clear surgical margins. Further, there is no serosal tissue surrounding the rectum. For all these reasons, preoperative Radiation Therapy (RT) with concurrent fluoropyrimidine based chemotherapy as a radiosensitizer followed by postoperative chemotherapy (total of 6 months of perioperative chemotherapy) has been the standard intervention. Infusional 5 Fluorouracil (5-FU) is often incorporated with concurrent radiation. This however is cumbersome and inconvenient for the patients. The NSABP protocol R-04 trial is a four arm phase III trial in which 1608 patients with clinical stage II or III rectal cancer undergoing preoperative RT were randomly assigned to one of four chemotherapy regimens – Continuous Infusion (CI) 5-FU 225mg/m2 over 24 hours, 5 days a week x 5 weeks (N=477), CI 5-FU with IV Oxaliplatin (ELOXATIN®) 50mg/m2 /wk x 5 weeks (N=329), Capecitabine (XELODA®) 825 mg/m2 PO BID 5 days/wk x 5 weeks (N=472) or XELODA® with ELOXATIN®, x 5 weeks (N=330). Radiation therapy consisted of 4,500cGy in 25 fractions over 5 wks plus a boost. The primary goals of this study were to compare preoperative XELODA® and CI 5-FU given along with concurrent pelvic RT and also determine whether ELOXATIN® would be of additional benefit. The primary endpoint of local-regional tumor control included locoregional tumor recurrence, less than complete surgical resection and no surgery. When combined with RT, this study showed no significant differences in local-regional tumor control, Disease Free Survival or Overall Survival between infusional 5-FU and XELODA® given alone or in combination with ELOXATIN®. The addition of ELOXATIN® was however associated with significantly more grade 3-4 diarrhea (P<0.0001). The authors concluded that outcomes and toxicities are similar with CI 5-FU or oral XELODA® when combined with RT. The addition of ELOXATIN® did not improve outcomes but resulted in significant toxicity. Oral XELODA® therefore obviates the need for central venous access and ambulatory infusion pumps and makes it more convenient for the patients without compromising efficacy. Allegra CJ, Yothers G, O'Connell MJ, et al. J Clin Oncol 32, 2014 (suppl 3; abstr 390)
Abiraterone acetate plus prednisone versus prednisone alone in chemotherapy-naive men with metastatic castration-resistant prostate cancer patient-reported outcome results of a randomised phase 3 trial
SUMMARY: Prostate Cancer is the most common cancer in American men and approximately 233,000 new cases will be diagnosed in 2014 and close to 30,000 men will die of the disease. The primary systemic intervention for patients with advanced prostate cancer is Androgen Deprivation Therapy (ADT). This can be accomplished by either surgical castration (bilateral orchicetomy) or medical castration, using LHRH (GnRH- Gonadotropin-Releasing Hormone) agonists. Majority of these patients will eventually develop progressive disease (Castrate Resistant Prostate cancer – CRPC), due to enhanced autocrine and /or paracrine synthesis of androgens or androgen precursors in the tumor micro environment. This has lead to the development of novel compounds that decrease androgen synthesis as well as androgen signaling in patients with CRPC.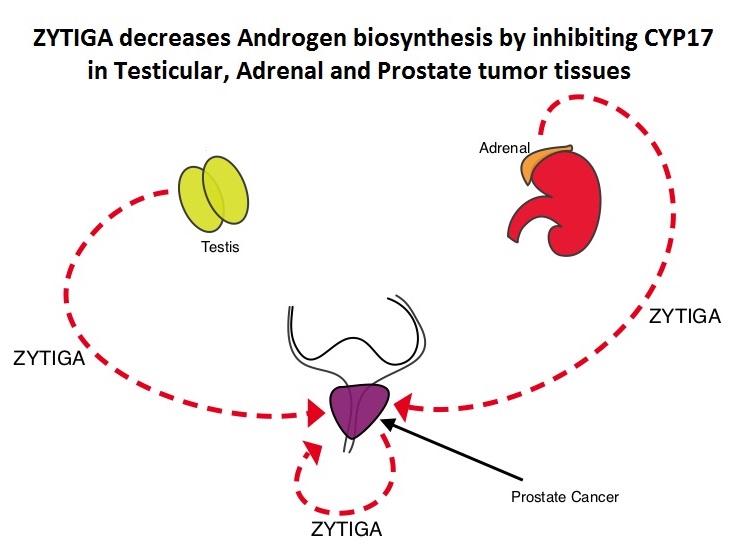 Abiraterone acetate (ZYTIGA®) is a novel, targeted, oral androgen biosynthesis inhibitor that decreases androgen production in the adrenal glands, testes and prostate cancer cells by inhibiting a steroidal enzyme CYP17A. Phase III trials have demonstrated that treatment with ZYTIGA® prolongs overall survival in metastatic CRPC patients, who had progressed after TAXOTERE® (Docetaxel) therapy, as well as those who are chemotherapy naive. ZYTIGA® delays deterioration of performance status, progression of fatigue and pain as well as development of skeletal related events, in TAXOTERE® refractory patients. It is important that any treatment considered for patients with asymptomatic or mildly symptomatic CRPC improves overall survival without negatively impacting Quality of Life. To address this further, the authors analyzed patient reported data related to pain and Quality of Life from a large randomized clinical trial. Of the 1088 chemotherapy-naïve, asymptomatic or mildly symptomatic CRPC patients randomized in this double-blind study, 546 patients received ZYTIGA® 1000 mg PO plus prednisone 5 mg twice daily and 542 patients received placebo plus prednisone. At the time of the planned interim analysis, ZYTIGA® improved radiographic progression-free survival, overall survival, and significantly delayed the initiation of chemotherapy. The authors in this publication reported the data related to pain and Quality of Life of these patients, at the time of the second preplanned interim analysis. Pain was assessed with the Brief Pain Inventory-Short Form (BPI-SF) questionnaire, which is a validated instrument to assess pain and Health Related Quality of Life (HRQoL) was measured with the Functional Assessment of Cancer Therapy—Prostate (FACT-P) questionnaire, which is a validated tool for metastatic CRPC. At a median follow-up of 22.2 months, the median time to progression of pain intensity was longer in patients receiving ZYTIGA® plus prednisone vs placebo plus prednisone (26.7 months vs 18.4 months, HR=0.82, P=0.049). The median time for pain to progress and interfere with daily activities was 10.3 months for ZYTIGA® vs 7.4 months for placebo (HR= 0.79, P=0.005). The median time to deterioration of HRQoL was longer in patients receiving ZYTIGA® plus prednisone vs those receiving placebo plus prednisone, as assessed by the FACT-P total score (12.7 months vs 8.3 months, HR=0.78, P=0.003). The authors concluded that ZYTIGA® given along with prednisone delays patient-reported pain progression and deterioration of HRQol, in chemotherapy-naive patients with metastatic CRPC, without compromising efficacy. Basch E, Autio K, Ryan CJ, et al. The Lancet Oncology 2013;14:1193 -1199
Abiraterone acetate (ZYTIGA®) is a novel, targeted, oral androgen biosynthesis inhibitor that decreases androgen production in the adrenal glands, testes and prostate cancer cells by inhibiting a steroidal enzyme CYP17A. Phase III trials have demonstrated that treatment with ZYTIGA® prolongs overall survival in metastatic CRPC patients, who had progressed after TAXOTERE® (Docetaxel) therapy, as well as those who are chemotherapy naive. ZYTIGA® delays deterioration of performance status, progression of fatigue and pain as well as development of skeletal related events, in TAXOTERE® refractory patients. It is important that any treatment considered for patients with asymptomatic or mildly symptomatic CRPC improves overall survival without negatively impacting Quality of Life. To address this further, the authors analyzed patient reported data related to pain and Quality of Life from a large randomized clinical trial. Of the 1088 chemotherapy-naïve, asymptomatic or mildly symptomatic CRPC patients randomized in this double-blind study, 546 patients received ZYTIGA® 1000 mg PO plus prednisone 5 mg twice daily and 542 patients received placebo plus prednisone. At the time of the planned interim analysis, ZYTIGA® improved radiographic progression-free survival, overall survival, and significantly delayed the initiation of chemotherapy. The authors in this publication reported the data related to pain and Quality of Life of these patients, at the time of the second preplanned interim analysis. Pain was assessed with the Brief Pain Inventory-Short Form (BPI-SF) questionnaire, which is a validated instrument to assess pain and Health Related Quality of Life (HRQoL) was measured with the Functional Assessment of Cancer Therapy—Prostate (FACT-P) questionnaire, which is a validated tool for metastatic CRPC. At a median follow-up of 22.2 months, the median time to progression of pain intensity was longer in patients receiving ZYTIGA® plus prednisone vs placebo plus prednisone (26.7 months vs 18.4 months, HR=0.82, P=0.049). The median time for pain to progress and interfere with daily activities was 10.3 months for ZYTIGA® vs 7.4 months for placebo (HR= 0.79, P=0.005). The median time to deterioration of HRQoL was longer in patients receiving ZYTIGA® plus prednisone vs those receiving placebo plus prednisone, as assessed by the FACT-P total score (12.7 months vs 8.3 months, HR=0.78, P=0.003). The authors concluded that ZYTIGA® given along with prednisone delays patient-reported pain progression and deterioration of HRQol, in chemotherapy-naive patients with metastatic CRPC, without compromising efficacy. Basch E, Autio K, Ryan CJ, et al. The Lancet Oncology 2013;14:1193 -1199
Rapid Increase in Breast Magnetic Resonance Imaging Use Trends From 2000 to 2011
SUMMARY: Breast cancer is the most common cancer among women in the United States and 1 in 8 women will develop invasive breast cancer during their lifetime. Screening mammography complemented by breast self exam and clinical breast exam has resulted in early detection of breast cancer and successful outcomes. Even though mammography is a sensitive screening test, a small percentage of breast cancers may not show up on mammograms but may be palpable on examination by the patient or the clinician. Further, mammograms are less likely to find breast tumors in younger women with dense breast tissue. A breast Magnetic Resonance Imaging (MRI) is more sensitive than mammography although the specificity of a breast MRI is lower, resulting in a higher rate of false-positive findings and potentially unnecessary biopsies. Microcalcifications in the breast can be missed by a breast MRI. Taking these factors into consideration, appropriate utilization of breast MRI becomes relevant.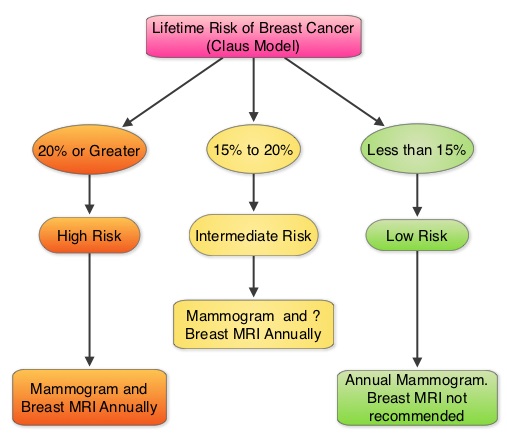
 The American Cancer Society (ACS) recommends an annual MRI as an adjunct to screening mammogram and clinical breast exam in certain groups with increased risk of breast cancer (See Figures). The authors conducted this study to determine the utilization of breast (MRI) in community settings. In this retrospective study, the authors reviewed data on 10,518 women from a not-for-profit health plan, and these women had at least one breast MRI between January 2000 and December 2011. The appropriateness of a breast MRI was determined using a prediction model obtained from electronic medical records on a subset of patients. Between 2000 and 2009, there was a 20-fold increase in the use of breast MRI from 6.5 per 10,000 women in the year 2000 to 130.7 per 10,000 in 2009. This increase then declined and stabilized to 104.8 per 10,000 by 2011. With regards to indications for a breast MRI, 51.7% had a family history of breast cancer, 30.1% had a personal history of breast cancer and 3.5% of women had a documented genetic mutation. It is interesting to note that of those who received screening or surveillance breast MRI’s, only 21% fulfilled the American Cancer Society (ACS) criteria for a breast MRI. Conversely, fewer participants (48.4%), with documented deleterious genetic mutations, received breast MRI screening. The authors concluded that breast MRI was over utilized in those who did not fit the ACS criteria and was under utilized in those with documented genetic mutations. It is their opinion that routine breast MRI screening is not recommended for a new breast cancer diagnosis or for breast cancer surveillance and should only be considered for the group of individuals who have the most benefit. Breast MRI is performed preferably between days 7-15 of menstrual cycle for premenopausal women, using a dedicated breast coil, with the ability to perform a biopsy under MRI guidance by experienced radiologists, during the same visit. Stout NK, Nekhlyudov L, Li L, et al. JAMA Intern Med. 2014;174:114-121.
The American Cancer Society (ACS) recommends an annual MRI as an adjunct to screening mammogram and clinical breast exam in certain groups with increased risk of breast cancer (See Figures). The authors conducted this study to determine the utilization of breast (MRI) in community settings. In this retrospective study, the authors reviewed data on 10,518 women from a not-for-profit health plan, and these women had at least one breast MRI between January 2000 and December 2011. The appropriateness of a breast MRI was determined using a prediction model obtained from electronic medical records on a subset of patients. Between 2000 and 2009, there was a 20-fold increase in the use of breast MRI from 6.5 per 10,000 women in the year 2000 to 130.7 per 10,000 in 2009. This increase then declined and stabilized to 104.8 per 10,000 by 2011. With regards to indications for a breast MRI, 51.7% had a family history of breast cancer, 30.1% had a personal history of breast cancer and 3.5% of women had a documented genetic mutation. It is interesting to note that of those who received screening or surveillance breast MRI’s, only 21% fulfilled the American Cancer Society (ACS) criteria for a breast MRI. Conversely, fewer participants (48.4%), with documented deleterious genetic mutations, received breast MRI screening. The authors concluded that breast MRI was over utilized in those who did not fit the ACS criteria and was under utilized in those with documented genetic mutations. It is their opinion that routine breast MRI screening is not recommended for a new breast cancer diagnosis or for breast cancer surveillance and should only be considered for the group of individuals who have the most benefit. Breast MRI is performed preferably between days 7-15 of menstrual cycle for premenopausal women, using a dedicated breast coil, with the ability to perform a biopsy under MRI guidance by experienced radiologists, during the same visit. Stout NK, Nekhlyudov L, Li L, et al. JAMA Intern Med. 2014;174:114-121.

Definitive chemoradiotherapy with FOLFOX versus fluorouracil and cisplatin in patients with oesophageal cancer (PRODIGE5/ACCORD17) final results of a randomised, phase 2/3 trial
SUMMARY: It is estimated that in 2014, over 18,000 new cases of esophageal carcinoma will be diagnosed in the U.S. and over 15,000 will die of the disease. There has been a rise in the incidence of esophageal cancer in recent decades. Even though stage 0, I, and II and most stage III esophageal cancers are potentially resectable, a significant number of these patients have associated comorbid conditions that may preclude them from undergoing surgical intervention. In this group of patients, as well as those with inoperable esophageal cancer, cisplatin based chemoradiation treatment has been associated with improved survival. Cisplatin however is associated with significant toxicities. The rationale for substituting ELOXATIN® for Cisplatin is based on its lower emetogenicity, lack of nephrotoxicity and lack of need for IV hydration. Prior phase II trials have demonstrated that ELOXATIN® (Oxaliplatin) based chemotherapy given alone or in combination with radiation therapy improved response rates with acceptable toxicities, in patients with advanced esophageal cancer. Based on this information, the authors conducted an open labeled, multicenter study to assess the efficacy and safety of the FOLFOX chemotherapy regimen (Fluorouracil plus Leucovorin and Oxaliplatin) compared to Fluorouracil and Cisplatin, when administered as a part of chemoradiotherapy treatment, in patients with locally advanced esophageal cancer. Patients with stage I—IVA esophageal carcinoma (adenocarcinoma, squamous-cell, or adenosquamous) who were not candidates for surgical intervention were randomly assigned to receive FOLFOX chemotherapy (N=131) or Cisplatin and Fluorouracil (N=128), with concurrent radiation. FOLFOX chemotherapy consisted of 6 cycles of ELOXATIN® 85 mg/m2 IV, Leucovorin 200 mg/m2 IV, Fluorouracil 400 mg/m2 IV bolus given on day 1, and infusional Fluorouracil 1600 mg/m2 given over 46 hours, every 2 weeks, with the first 3 cycles given concurrently with radiation therapy. Chemotherapy with Cisplatin and Fluorouracil consisted of 4 cycles of Cisplatin 75 mg/m2 IV given on day 1 and infusional Fluorouracil 1000 mg/m2 per day, given for 4 days, with the first 2 cycles given concurrently with radiation therapy at 4 week intervals and the remaining 2 cycles given 3 weeks apart after completion of radiation therapy. Both treatment groups received 50Gy radiotherapy, in 25 fractions, at five fractions per week. The primary endpoint was Progression Free Survival (PFS). At a median follow up of 25.3 months, the median PFS was 9.7 months in the FOLFOX group and 9.4 months in the Cisplatin group and this was not statistically significant (P=0.64), suggesting that FOLFOX in combination with radiation may be an alternative to Cisplatin and Fluorouracil. FOLFOX chemotherapy may alleviate Cisplatin related toxicities such as nausea and vomiting, nephrotoxicity and the need for IV hydration, making this a much more tolerable regimen in advanced esophageal carcinoma. Conroy T, Galais M, Raoul J, et al. Lancet Oncol, 2014;15: 305-314
