SUMMARY: It is estimated that in the United States, more than 12,000 people are diagnosed with a Neuroendocrine tumor each year. NeuroEndocrine Tumors (NETs) arise from cells of the endocrine and nervous systems and produce biogenic amines and polypeptide hormones. NETs can be clinically symptomatic (functioning) or silent (nonfunctioning). The incidence is higher in African-Americans and the most common sites of NETs are the lung, stomach, appendix, cecum, duodenum, pancreas, jejunum/ileum, colon, and rectum. NeuroEndocrine Tumors originating in the gastrointestinal tract and pancreas are also known as GastroEnteroPancreatic NETs (GEP-NETs). They constitute about 2% of all neoplasms and account for about 50-70% of all NETs. They are more frequent in gastric fundus/body, proximal duodenum, Vater’s papilla, pancreas, tip of the appendix, terminal ileum, and lower rectum. Majority of GEP-NETs are not symptomatic (nonfunctioning tumors), difficult to diagnose, and present with advanced disease at initial diagnosis. They often metastasize to the mesentery, peritoneum and liver. The functioning tumors however secrete biologically active substances that can lead to the development of characteristic clinical syndromes. NeuroEndocrine Tumors may be sporadic or may be a component of inherited genetic syndromes such as Multiple Endocrine Neoplasia (MEN) types 1 and 2. Most NETs are classified based on tumor differentiation into 1) Well-differentiated, Low-grade (G1) 2) Well-differentiated, Intermediate-grade (G2) and 3) Poorly differentiated, High-grade (G3). Tumor differentiation and tumor grade often correlate with mitotic count and Ki-67 proliferation index. Even though surgery is curative when the tumor is detected early, this is often not the case, as most patients present with metastatic disease at the time of diagnosis.
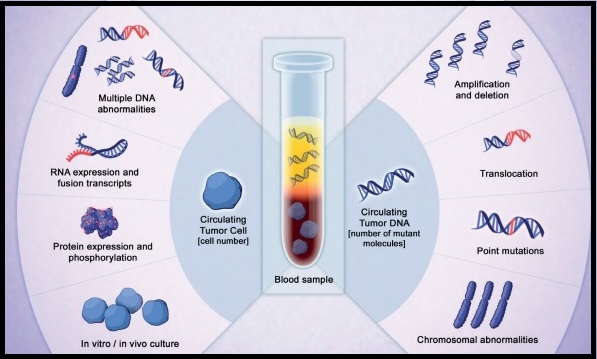
Chromogranin A is a glycoprotein precursor to several functional peptides and is considered a standard biomarker for NETs. However, serum Chromogranin A levels can be elevated in several non-oncologic conditions such as atrophic gastritis, pancreatitis, chronic hepatitis, liver cirrhosis, irritable bowel, and inflammatory bowel diseases. The use of proton pump inhibitors can also result in elevated Chromogranin A levels. Diagnostic imaging as well as serum biomarkers lack the sensitivity and are unable to detect early changes in disease state. As such, the absence of a clinically useful blood biomarker remains an important unmet need.
The NETest® is a novel blood-based (liquid biopsy) molecular diagnostic test intended to aid in the identification of neuroendocrine tumor disease activity. The assay involves measurement of 51 neuroendocrine tumor gene transcripts, by Polymerase Chain Reaction (PCR). The gene expression signatures, which is the tumor activity score, stratifies patients into three groups: low score (40% or less), moderate/intermediate score (41-79%) and high score (80% or more). A higher score at the time of testing indicates a higher risk of tumor activity. Previously published prospective clinical studies have demonstrated the value of NETest® in predicting the effectiveness of surgery, in its ability to monitor tumor progression during SomatoStatin Analog (SSA) therapy, in its utility for watchâ€andâ€wait programs, as well as its ability in predicting response to Peptide Receptor RadioTherapy (PRRT) prior to treatment initiation.
The authors in this study examined the clinical utility of NETest® multigene assay in a realâ€world setting, utilizing a registry of NETs in the USA. This registry was established to include clinical and biomarker data from patients enrolled by interested physicians who could then use it to answer specific clinical questions. NETest® registry patients were evaluated from large referral practices, and their subsequent clinical data, including decisionâ€making, were interfaced with NETest® data. This study addressed five important questions: 1) What is the diagnostic accuracy of the NETest®? 2) Does the NETest® score accurately reflect the disease status? 3) Does it have clinical utility in decisionâ€making? 4) Can it alter the frequency and type of imaging? 5) Does the NETest® have greater clinical utility than Chromogranin A?. The diagnostic accuracy and relationship to clinical disease status were evaluated in two patient cohorts (treated and watchâ€andâ€wait).
A total of 100 patients with pathological confirmation of a NET were enrolled over a 22 month period and NETest® was performed at enrollment. The primary site of the NET was gastroenteropancreatic (68%), lung 20%, and of unknown origin (12%). Stage IV disease was present in 96% of patients, 70% had undergone surgery before enrollment, 97% had wellâ€differentiated, lowâ€grade tumors and 56% were on drug therapy. The median age was 62 years and the median follow up was 6 months.
The diagnostic accuracy of NETest® was more than 96% and the NETest® was concordant with imageâ€confirmed disease in 96% of patients. Scores were reproducible (97%) and concordant with clinical status (98%). Chromogranin A was ordered for 53 of the 100 patients, but was not elevated in 75% of these patients despite documented clinical evidence of disease. NETest® was positive in 100% of these patients (P=0.0004 for accuracy). NETest® scores were reproducible (97%) and concordant with clinical status (98%). Multivariate analyses identified the NETest® score as the only variable significantly related to Progression Free Survival (PFS). High NETest® score correlated with progressive disease (81%; median PFS, 6 months), and low NETest® score correlated with stable disease (87%; median PFS, Not Reached)-P<0.0001). The NETest® score was the only feature linked to PFS (odds ratio, 6.1; p < .0001). In the watchâ€andâ€wait group of patients, low NETest® scores were concordant with stable disease in 100% of patients, and high NETest® scores were associated with management changes in 83% of patients. In the treated group, all patients with low NETest® scores (100%) remained stable. A high NETest® score was linked to treatment intervention and disease stabilization (100%). Further, the utilization of NETest® was associated with reduced imaging (biannual to annual) in 36-38% of patients.
It was concluded that realâ€time liquid biopsy assessment of Neuroendocrine tumors with NETest® has more than 96% diagnostic accuracy, and has clinical utility in monitoring disease status, as well as patient management. Assessment of NETest Clinical Utility in a U.S. Registryâ€Based Study. Liu E, Paulson S, Gulati A, et al. The Oncologist 2019;24:783-790.