SUMMARY: The Center for Disease Control and Prevention (CDC) estimates that approximately 1-2 per 1000 individuals develop Deep Vein Thrombosis/Pulmonary Embolism (PE) each year in the United States, resulting in 60,000 – 100,000 deaths. VTE is the third leading cause of cardiovascular mortality with a mortality rate of up to 25% in those with untreated acute pulmonary embolism. Even though the risk of recurrent VTE is high after anticoagulant treatment is discontinued in patients with a first unprovoked venous thromboembolism (10-30% risk of a recurrence within 5 years following cessation of anticoagulation), a significant number of these patients receive therapy for 6-12 months and are not routinely treated with long term anticoagulant therapy. This may be due to bleeding risks, cost of therapy and need for diligent monitoring while on long term anticoagulation. 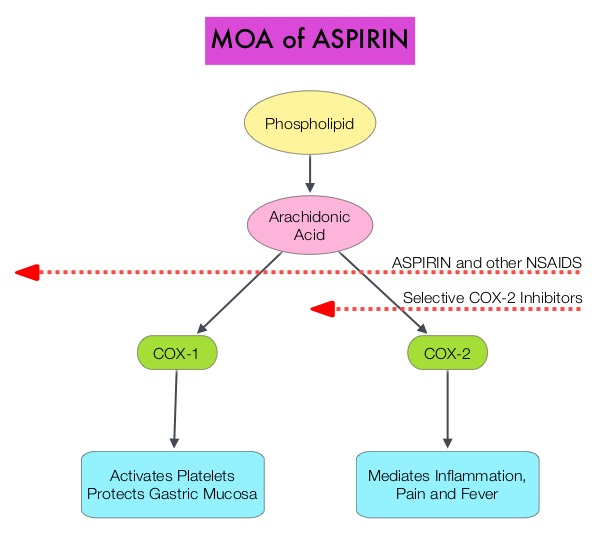 Aspirin is a non-selective, irreversible inhibitor of both COX-1 and COX-2 (Cyclooxygenases 1 and 2). It inhibits the production of Prostaglandins and Thromboxane A2 and there by decreases platelet aggregation. Both ASPIRE and WARFASA trials support the role of aspirin for the prevention of recurrent VTE in patients with an unprovoked VTE, after 6-18 months of anticoagulation therapy. These trials however were not individually powered to detect benefits of treatment for particular outcomes or subgroups of patients. The INSPIRE Collaboration involved further analysis of these trials to detect outcomes in pre-specified subgroups of patients. The intent-to-treat analysis included 1,224 patients and at a median follow up of 30.4 months, daily Aspirin given at a dose of 100mg reduced recurrent VTE events by 32% (HR=0.68; P=0.008) and this included reduction in recurrent Deep Vein Thrombosis by 34% (HR=0.66; P=0.01) and Pulmonary Embolism by 34% (HR=0.66; P=0.08), compared to Placebo. After adjustment for treatment adherence, recurrent VTE was reduced by 42% (HR=0.58; P=0.005). Subgroup analyses indicated similar relative, but larger absolute, risk reductions in men and older patients. Aspirin also reduced major vascular events by 44% (HR=0.66; P=0.002). The major bleeding rate was low at 0.5%/year for Aspirin and 0.4%/year for Placebo. The authors concluded that aspirin reduces the risk of recurrent VTE. Even though the efficacy of aspirin is inferior to that of Warfarin or the new oral anticoagulants, this data suggests that Aspirin should be strongly considered in patients with unprovoked VTE for whom long-term anticoagulation therapy with Warfarin or one of the new oral anticoagulants has to be discontinued or is not an appropriate option. Aspirin however, should not be considered a replacement option for conventional anticoagulation. Simes J, Becattini C, Agnelli G, et al. Circulation. 2014; 130:1062-1071
Aspirin is a non-selective, irreversible inhibitor of both COX-1 and COX-2 (Cyclooxygenases 1 and 2). It inhibits the production of Prostaglandins and Thromboxane A2 and there by decreases platelet aggregation. Both ASPIRE and WARFASA trials support the role of aspirin for the prevention of recurrent VTE in patients with an unprovoked VTE, after 6-18 months of anticoagulation therapy. These trials however were not individually powered to detect benefits of treatment for particular outcomes or subgroups of patients. The INSPIRE Collaboration involved further analysis of these trials to detect outcomes in pre-specified subgroups of patients. The intent-to-treat analysis included 1,224 patients and at a median follow up of 30.4 months, daily Aspirin given at a dose of 100mg reduced recurrent VTE events by 32% (HR=0.68; P=0.008) and this included reduction in recurrent Deep Vein Thrombosis by 34% (HR=0.66; P=0.01) and Pulmonary Embolism by 34% (HR=0.66; P=0.08), compared to Placebo. After adjustment for treatment adherence, recurrent VTE was reduced by 42% (HR=0.58; P=0.005). Subgroup analyses indicated similar relative, but larger absolute, risk reductions in men and older patients. Aspirin also reduced major vascular events by 44% (HR=0.66; P=0.002). The major bleeding rate was low at 0.5%/year for Aspirin and 0.4%/year for Placebo. The authors concluded that aspirin reduces the risk of recurrent VTE. Even though the efficacy of aspirin is inferior to that of Warfarin or the new oral anticoagulants, this data suggests that Aspirin should be strongly considered in patients with unprovoked VTE for whom long-term anticoagulation therapy with Warfarin or one of the new oral anticoagulants has to be discontinued or is not an appropriate option. Aspirin however, should not be considered a replacement option for conventional anticoagulation. Simes J, Becattini C, Agnelli G, et al. Circulation. 2014; 130:1062-1071

