SUMMARY: Lynch Syndrome (Hereditary NonPolyposis Colorectal Cancer – HNPCC), is an autosomal dominant inherited disorder associated with increased risk of colorectal, endometrial, ovary, gastric, small bowel, pancreatic, brain, ureter or renal pelvis cancer. In the United States, approximately 140,000 new cases of colorectal cancer are diagnosed each year of which 3 to 5 percent are caused by Lynch Syndrome (LS). One in 35 patients with newly diagnosed colorectal cancer is related to Lynch Syndrome. Four genes, MLH1, MSH2, MSH6, and PMS2 are involved in the repair of mistakes that occur during DNA replication.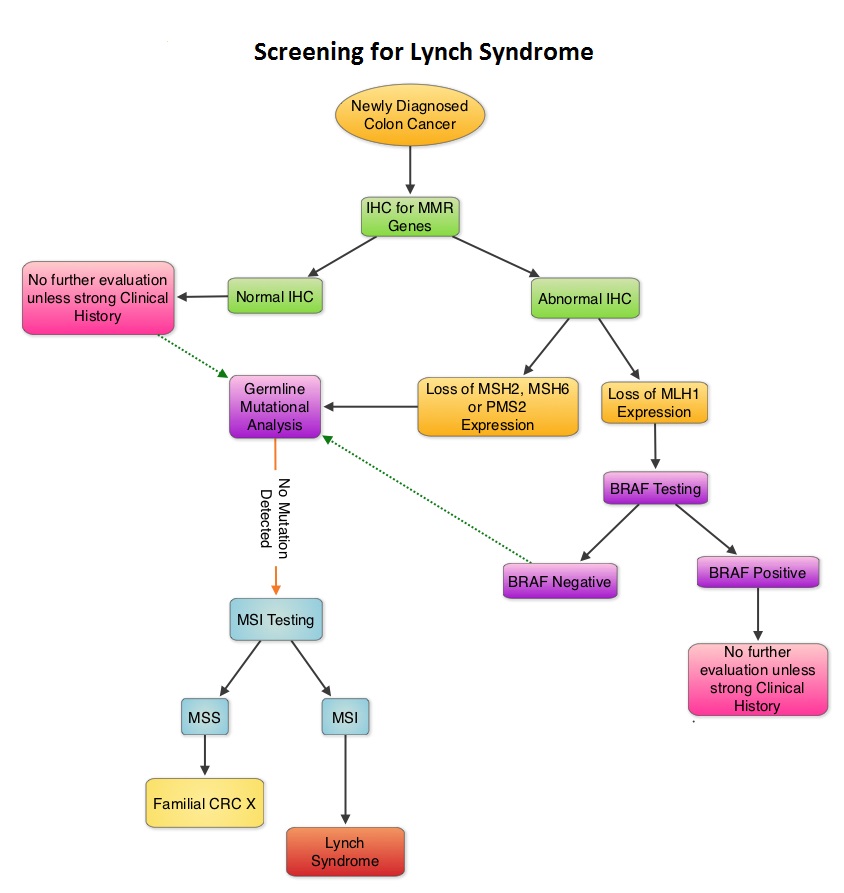 When any of these genes are mutated, repair of DNA replication mistakes is prevented resulting in continuous division of abnormal cells and possibly cancer. The EPCAM gene lies next to the MSH2 gene on chromosome 2 and mutations in the EPCAM gene can cause the MSH2 gene to be inactivated, interrupting DNA repair and leading to accumulation of DNA replication errors and possible malignancy. A Clinical Diagnosis of Lynch Syndrome can be made based on personal and family history if at least three relatives have a malignancy associated with Lynch Syndrome such as colorectal, endometrial, small bowel, ureter or renal pelvis cancer. In addition the following criteria should be met: • One relative must be a first-degree relative of the other two. • At least two successive generations must be affected. • At least one relative with a Lynch syndrome associated cancer should be diagnosed before 50 years of age. • Familial Adenomatous Polyposis should be excluded. • Tumors should be verified whenever possible. Because family history can sometimes be difficult to obtain or confirm NCCN in those circumstances has recommended screening all newly diagnosed colorectal cancer patients for Lynch syndrome. Germline defects/mutations in the mismatch repair genes MLH1, MSH2, MSH6 and PMS2 results in microsatellite instability in tumors. Tumors are described as MSI-High when they have changes in 2 or more, of the 5 microsatellite markers. So, High levels of MSI within a tumor are suggestive of defective DNA mismatch repair. ImmunoHistoChemistry (IHC) staining of tumor tissue is performed for protein expression of the four mismatch repair genes known to be mutated in Lynch Syndrome (MLH1, MSH2, MSH6 and PMS2). IHC test is described as normal when all 4 mismatch repair proteins are normally expressed suggesting that an underlying mismatch repair gene mutation is unlikely. When IHC test is abnormal, it means that that at least one of the 4 mismatch repair proteins is not expressed and an inherited mutation may be present in the gene related to that protein. This can be further confirmed by mutation analysis of the corresponding gene. Screening tests for Lynch syndrome include IHC staining of tumor tissue for protein expression of the four mismatch repair genes and tumor evaluation for MSI. In LS, more than 90% of the tumors are MSI-H (microsatellite instability-high) and/or lack expression of at least one of the mismatch repair proteins by IHC staining and there is a 96% correlation between IHC and MSI when used as a screening test for LS. Approximately 5% of tumors that display MSI may have normal protein expression for the four mismatch repair genes. It should be noted that an abnormal MSI and/or IHC test in colon cancer patients is not diagnostic of Lynch syndrome but can be a useful screening test. This is because even though MSI in the tumor tissue is pathognomonic of Lynch syndrome, approximately 15% of patients with sporadic colorectal cancers exhibit tumors with high MSI as a result of somatic MLH1 promoter hypermethylation. Further, the majority of colon cancer tumors that lack protein expression on IHC staining of MLH1 (often coexisting with loss of PMS2) are often due to an acquired genetic defect. If the IHC indicates absence of MLH1 protein expression, tumor should be tested for BRAF mutation V600E which can be seen in sporadic colorectal cancers but rarely found in patients who have Lynch Syndrome. Once a diagnosis of Lynch Syndrome is made, at risk family members should undergo colonoscopic evaluation at 20-25 years of age or 2-5 years prior to the earliest colon cancer, if it is diagnosed before age 25 and is repeated every 1-2 years. Prophylactic hysterectomy and bilateral salpingo-oophorectomy (BSO) should be considered by women who have completed childbearing. NCCN Guidelines Version 1.2014 Lynch Syndrome
When any of these genes are mutated, repair of DNA replication mistakes is prevented resulting in continuous division of abnormal cells and possibly cancer. The EPCAM gene lies next to the MSH2 gene on chromosome 2 and mutations in the EPCAM gene can cause the MSH2 gene to be inactivated, interrupting DNA repair and leading to accumulation of DNA replication errors and possible malignancy. A Clinical Diagnosis of Lynch Syndrome can be made based on personal and family history if at least three relatives have a malignancy associated with Lynch Syndrome such as colorectal, endometrial, small bowel, ureter or renal pelvis cancer. In addition the following criteria should be met: • One relative must be a first-degree relative of the other two. • At least two successive generations must be affected. • At least one relative with a Lynch syndrome associated cancer should be diagnosed before 50 years of age. • Familial Adenomatous Polyposis should be excluded. • Tumors should be verified whenever possible. Because family history can sometimes be difficult to obtain or confirm NCCN in those circumstances has recommended screening all newly diagnosed colorectal cancer patients for Lynch syndrome. Germline defects/mutations in the mismatch repair genes MLH1, MSH2, MSH6 and PMS2 results in microsatellite instability in tumors. Tumors are described as MSI-High when they have changes in 2 or more, of the 5 microsatellite markers. So, High levels of MSI within a tumor are suggestive of defective DNA mismatch repair. ImmunoHistoChemistry (IHC) staining of tumor tissue is performed for protein expression of the four mismatch repair genes known to be mutated in Lynch Syndrome (MLH1, MSH2, MSH6 and PMS2). IHC test is described as normal when all 4 mismatch repair proteins are normally expressed suggesting that an underlying mismatch repair gene mutation is unlikely. When IHC test is abnormal, it means that that at least one of the 4 mismatch repair proteins is not expressed and an inherited mutation may be present in the gene related to that protein. This can be further confirmed by mutation analysis of the corresponding gene. Screening tests for Lynch syndrome include IHC staining of tumor tissue for protein expression of the four mismatch repair genes and tumor evaluation for MSI. In LS, more than 90% of the tumors are MSI-H (microsatellite instability-high) and/or lack expression of at least one of the mismatch repair proteins by IHC staining and there is a 96% correlation between IHC and MSI when used as a screening test for LS. Approximately 5% of tumors that display MSI may have normal protein expression for the four mismatch repair genes. It should be noted that an abnormal MSI and/or IHC test in colon cancer patients is not diagnostic of Lynch syndrome but can be a useful screening test. This is because even though MSI in the tumor tissue is pathognomonic of Lynch syndrome, approximately 15% of patients with sporadic colorectal cancers exhibit tumors with high MSI as a result of somatic MLH1 promoter hypermethylation. Further, the majority of colon cancer tumors that lack protein expression on IHC staining of MLH1 (often coexisting with loss of PMS2) are often due to an acquired genetic defect. If the IHC indicates absence of MLH1 protein expression, tumor should be tested for BRAF mutation V600E which can be seen in sporadic colorectal cancers but rarely found in patients who have Lynch Syndrome. Once a diagnosis of Lynch Syndrome is made, at risk family members should undergo colonoscopic evaluation at 20-25 years of age or 2-5 years prior to the earliest colon cancer, if it is diagnosed before age 25 and is repeated every 1-2 years. Prophylactic hysterectomy and bilateral salpingo-oophorectomy (BSO) should be considered by women who have completed childbearing. NCCN Guidelines Version 1.2014 Lynch Syndrome

